Abstract
Introduction: In the last decades, it has been described the potential role of Nuclear SET domain (NSD) Protein Lysine Methyltransferases (KMT) family members (NSD1/KMT3B, NSD2/WHSC1/MMSET, and NSD3/WHSC1L1) in cancer development and progression, mostly associated with overexpression and poor prognosis. However, little is known about their impact on acute leukemia, especially in acute promyelocytic leukemia (APL). Even though the most important advance in APL was the therapy with ATRA, risk stratification remains an important issue. Besides the influence of molecular genetic markers into APL prognosis during the last years, risk stratification is predicted by leukocytes and platelet counts only. We aimed to evaluate the expression levels of NSD genes and their correlation with APL prognosis.
Methods: A total of 153 consecutive patients (age, 9-78y) with newly diagnosed APL who were enrolled in the IC-APL study were included. Details about the diagnosis, eligibility criteria and classification of patients are published elsewhere (Rego EM et al., Blood 2013). The treatment protocol was identical to that adopted in the PETHEMA/HOVON LPA2005 trial, except for the replacement of idarubicin by daunorubicin. For comparison purposes, isolated CD34+ cells (n=16), de novo core binding factor-leukemia (CBF-leukemia, 24 patients), cytogenetically normal-AML (CN-AML, 30 patients) and not otherwise specified AML (NOS-AML, 11 patients) were included. Gene expression profile was analyzed by qPCR using the normalized copy number to express the results. Using survival receiver operating characteristic (ROC) curve analysis and the C index, we dichotomized patients into two groups according to NSD1, 2 and3 expression using the median value as cut off (groups "lower" and "higher" expression).
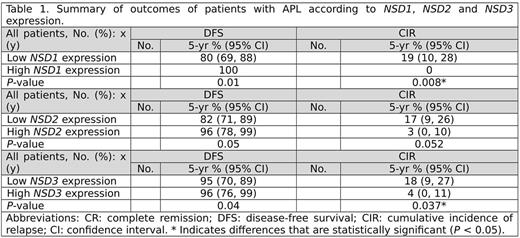
Results: NSD expression was lower in APL, CBF -leukemia, CN-AML, and NOS-AML compared to isolated CD34+ from healthy donor samples (P<.001). Restricting our analysis to APL patients, we show that lower NSD genes expression was associated with high-risk group, according to PETHEMA/GIMEMA criteria (NSD1, P=.007; NSD2, P=.022, and NSD3, P=.019). Baseline features were similar between patients with low and high NSD expression levels, except for high frequency of Bcr2 breakpoint in patients with high expression of NSD1 and NSD3 (P=.006 for both) and lower frequency of FLT3-ITD mutation in group with lower expression of NSD1 (OR:0.28; 95% CI: 0.07-0.9; P=.04). With a median of follow up of 32 months (1-101 months), the estimated 5y OS rate was 79% (95% CI: 72-84%). Patients with higher expression of NSD2 gene had higher 5y OS rate (84%, 95% CI: 71-91%) compared to lower expression group (53%, 95% CI: 23-73%) (HR: 0.21; 95% CI: 0.1-0.5; P<.0001) albeit these data were not supported by multivariate logistic regression analysis considering leukocyte count, age and gender as confounders (HR: 0.48; 95% CI: 0.18-1.3; P=.161). Overall, 126/153 (84%) patients achieved complete hematological remission (CR). The estimated 5y DFS and the CIR rates were 87% (95% CI: 80-92) and 12% (95% CI: 7-17%), respectively. According to NSD gene expression, patients with high expression had a higher 5y DFS rate than those with a lower expression (Table 1). In agreement CIR rate was higher in patients with lower NSD expression in comparison to patients with high expression (Table 1). .
Conclusion: This is the first study to show that the expression of NSD genes is decreased in APL. Our results show that low NSD transcript levels may predict a short survival and high risk of relapse in APL patients treated with ATRA and anthracycline-based chemotherapy.
Bittencourt: Janssen, Takeda: Honoraria. Pagnano: Roche: Speakers Bureau; Amgen: Consultancy; Novartis: Consultancy; Bristol-Meirs Squibb: Consultancy, Speakers Bureau. Lo Coco: Lundbeck: Honoraria, Speakers Bureau; TEVA: Honoraria, Speakers Bureau; Novartis: Honoraria, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal